The science behind our approach
The immune system is a real masterpiece that does extraordinary things every day while we do not realize such numerous activities. Over the past years it has turned out, that the immune system and inflammation play major roles in many medical fields and diseases, including oncology, cardiovascular diseases (CVD), diabetes, neurodegenerative diseases, rheumatological and autoimmune diseases; neuroimmune connections in aging are also well described.
The immune system is now recognized to be centrally involved in the vast majority of major neurological disorders including Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), stroke, epilepsy, traumatic brain injury, glioblastoma, mental illness, autism, pain, and addiction just to name a few. Even less brain-centric disorders like obesity, cardiovascular disease, and intestinal disorders are now recognized to be highly influenced by neuroimmunology via the microbiome-neuroimmune and the vagus nerve-neuroimmune axes.
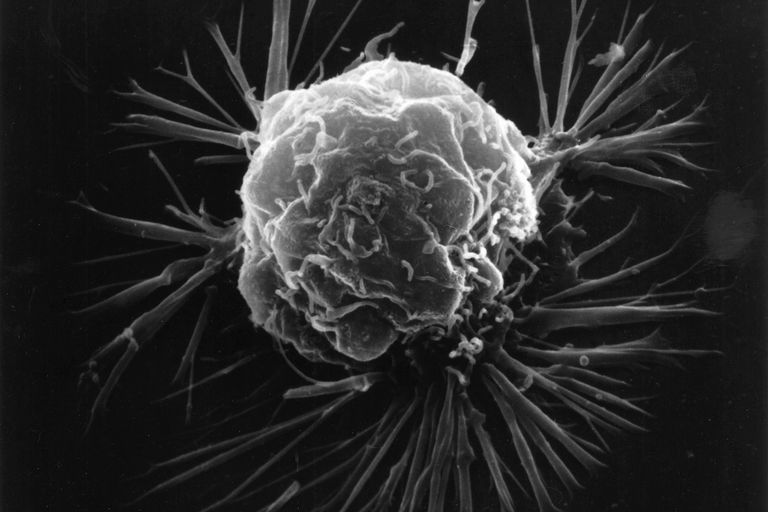
Oncology
Despite tumor development is the result of genetic derangement, it is the immune system that plays a critical role in tumor prevention, and in production (pathogenesis, surveillance, progression, and treatment of solid tumors).
The ability to evade immune-mediated destruction has been described as a shared trait across multiple tumor types. Thus, cancer is characterized by an immunological imbalance that goes beyond the primary tumor.
Autoimmune diseases
Autoimmune disorders are conditions in which the immune system is unable to differentiate between healthy tissue and potentially harmful antigens. Nearly 100 distinct autoimmune diseases have been identified to date.
Autoimmune diseases particularly benefit from analyzing real-world data as clinical trials struggle to recruit enough patients in a realistic amount of time. Most disease types are chronic, which is why longitudinal datasets are required - trials are just too short.
Cardiovascular diseases (CVD)
Over the past two decades, the emerging field of cardioimmunology has demonstrated how cells of the immune system play vital roles in the pathogenesis of CVD.
Inflammation and fibrosis are hallmarks of tissue repair process and organ failure progression in cardiovascular diseases.
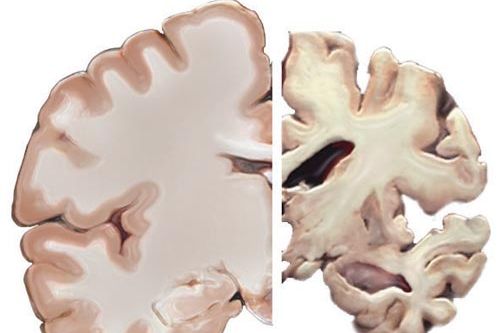
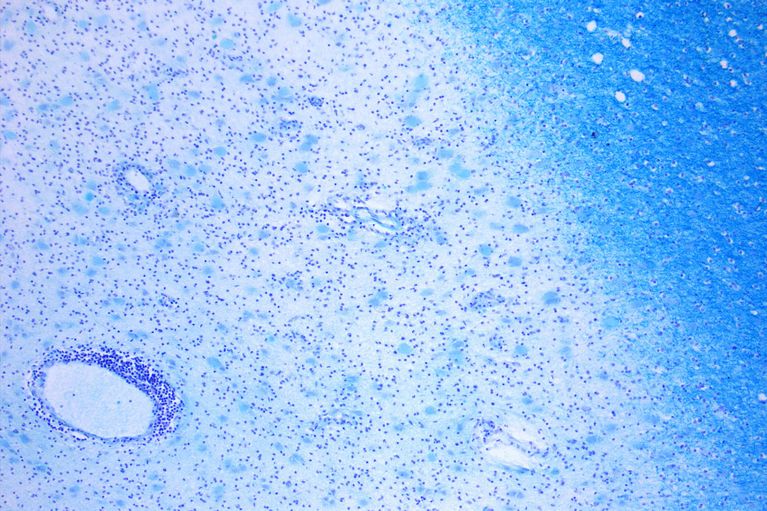
Neurodegenerative diseases
For decades, the brain was thought to be an immune-privileged organ, physically separated from the immune system.
Emerging evidence now points to critical roles forvimmunology in almost every facet of fundamental neurobiology including normal brain development, cognition, and behavioral control.
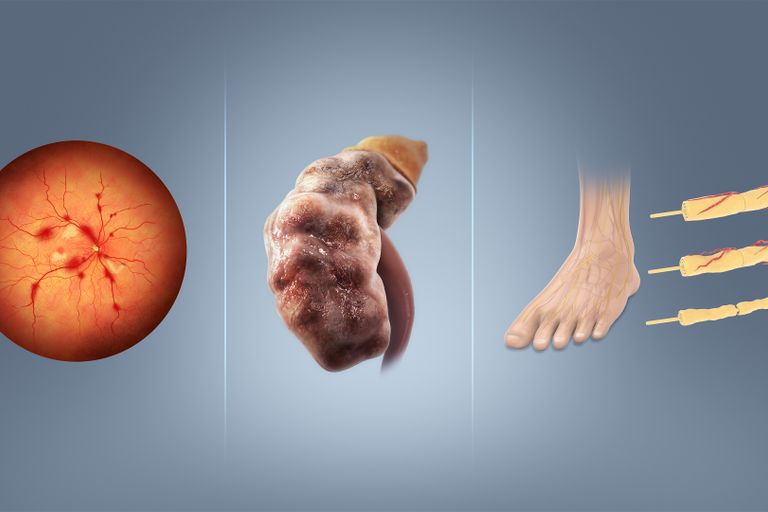
Diabetes
If you are into diabetes you are definitely also into immune system it is a typical metabolic inflammatory disease. Metabolic abnormalities are important drivers of the induction and progression of type 2 diabetes mellitus (T2DM). A bidirectional interaction between metabolism and immune system was found in analysis of the immunometabolism. Inflammation boosts metabolic abnormalities (e.g. obesity and T2D), while metabolic factors, regulate immune cell functions.
Diabetics have an increased risk of cancer. That's why R&D can hardly avoid the triangle of immunesystem, immunotherapy and antidiabetic drugs.

Aging & Longevity
Among other variables immune memory limits human longevity.
When it comes to health and longevity, the "age" of one's immune system most certainly outperforms the chronological age. On average, centenarians have an immune age that is 40 years younger than what is considered 'normal'.
Age-related pathologies are attributed to potentially most of all morbidities. Loss of power of the immune system, termed immunosenescence, correlates with decreased vaccination responses and increased incidence and severity of infectious disease.
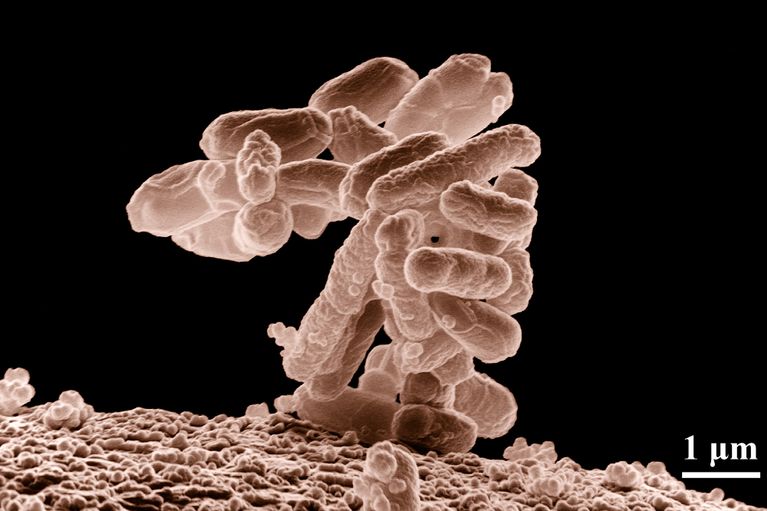
Multi-omics: microbiome
There has been an exponential increase in the number of studies investigating associations of microbiome and cancer, from oncogenesis and cancer progression to resistance or sensitivity to specific anticancer therapies. The gut microbiome is now known to play a significant role in antitumor immune responses and in predicting the efficacy of immune-checkpoint inhibitors in cancer patients.
Recently an analysis of 35 tumor types found correlations with intratumor fungi in some tumor-types and patient outcome in immunotherapy.
Gut microbial communities are capable of enzymatically transforming pharmaceutical compouns into active, inactive, and toxic metabolites, thus potentially affecting the pharmacokinetics and bioavailability of orally administered medications.
Why do both new and approved drugs only work for some patients? The stakes are high for patients, healthcare systems, investors and pharma / biotech. Recent evidence suggests a role for the gut microbiome. While the initial focus was on bacteria, now viruses (as part of the gut microbiota) are beginning to appear on the radar. Bacteriophages are virus that infect and replicate within bacteria and archaea.